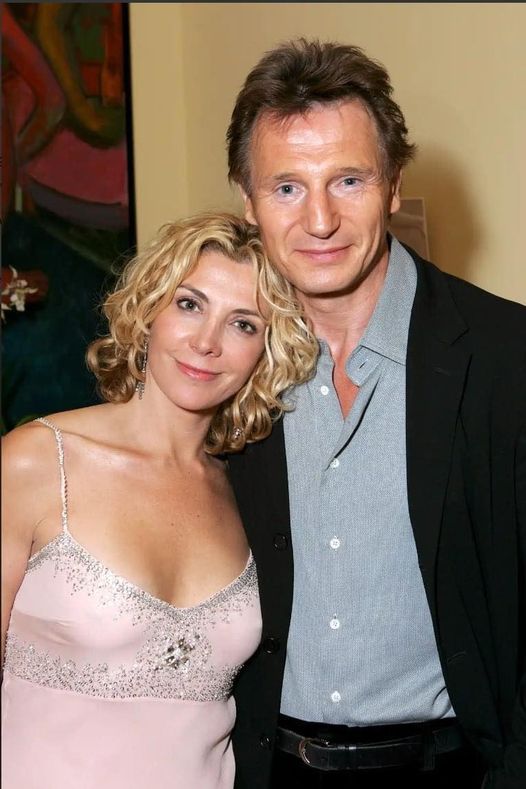
That Anna Christie Broadway play from 1993 was a serendipitous moment for a Hollywood couple that taught us what true love is. It was the play that brought Liam Neeson and Natasha Richardson together.
At the time, Richardson was married to producer Robert Fox, but meeting Neeson made her fall for him with the same passion he fell for her.
Unfortunately, Richardson passed away in 2009, and Neeson never married again. Years after loosing her, the Taken star still grieves for the woman who stole his heart forever.
Speaking of the moment he first met her, Neeson told Anderson Cooper on 60 Minutes: “She was a radiant beauty. Yeah, cascading hair. I remember. There was—that was very, very attractive. I’d never had that kind of an explosive chemistry situation with an actor, or actress.” He then continued saying: “We had just this wonderful kind of dance—free dance on stage every night. She and I were like [Fred] Astaire and [Ginger] Rogers.”
At the time of her death, the couple’s sons, Micheal and Daniel, were 13 and 12 years old.
Who is at Risk for Pre-Diabetes?
Pre-diabetes, a precursor to type 2 diabetes, can affect anyone. However, certain factors increase the risk of developing this condition. By understanding these risk factors, individuals can take proactive measures to prevent or manage pre-diabetes.
Advertisements
Factors Increasing Development Of Pre-Diabetes:
Being overweight: Excess body weight puts additional strain on the body’s ability to use insulin effectively.
Family history of type 2 diabetes: If close relatives have been diagnosed with type 2 diabetes, the risk of developing pre-diabetes is higher.
Age over 45: As we age, the risk of developing insulin resistance and pre-diabetes increases.
Having African, Latino, or Native American ancestry: Certain ethnicities have a higher risk of developing pre-diabetes.
Smoking: Smoking cigarettes can increase insulin resistance, making the development of pre-diabetes more likely.
Taking certain medications: Certain medications, such as steroids and anti-psychotics, can contribute to insulin resistance and increase the risk of pre-diabetes.
Medical Conditions Associated With Insulin Resistance:
Obstructive sleep apnea: Sleep apnea has been linked to insulin resistance and an increased risk of pre-diabetes.
Fatty liver disease: Non-alcoholic fatty liver disease can lead to insulin resistance and pre-diabetes.
Polycystic ovarian syndrome (PCOS): Women with PCOS have a higher risk of insulin resistance and pre-diabetes.
Cushing’s syndrome: This hormonal disorder can increase the risk of developing pre-diabetes.
Lipodystrophy syndromes: These rare disorders affect fat storage and can contribute to insulin resistance.
By identifying these risk factors and taking preventive measures, individuals can reduce the likelihood of developing pre-diabetes. Regular check-ups and monitoring of blood sugar levels are also essential for individuals at risk.
Recognizing Pre-Diabetes Symptoms
The symptoms of pre-diabetes are often subtle, and many individuals may not experience any symptoms at all. However, there are certain signs that can indicate the presence of insulin resistance. By being aware of these symptoms, individuals can seek medical attention for diagnosis and early intervention.
Physical Signs and Measurements
If you notice any of the following physical signs or measurements, it could be an indication of pre-diabetes:
A waistline over 40 inches in men and over 35 inches in women
Skin tags or patches of dark velvety skin called acanthosis nigricans
High blood pressure
Elevated fasting glucose levels
Increased triglycerides
Low HDL cholesterol
These signs may not be exclusive to pre-diabetes and can be related to other health conditions. Therefore, it is important to consult with a healthcare professional for a proper diagnosis.
Common Pre-Diabetes Symptoms
In addition to physical signs, individuals with pre-diabetes may experience the following symptoms:
Frequent urination
Excessive thirst
Unexplained weight loss
While these symptoms can be attributed to various factors, it is essential to be aware of them and discuss them with a healthcare professional to rule out pre-diabetes as a potential cause.

Alright, imagine you’re about to start a big adventure, like stepping into a magical world filled with books, new friends, and exciting discoveries. That’s what happened to Alex on their first day at university.
Alex had butterflies fluttering in their stomach as they walked through the gates of the university, feeling a mix of excitement and nervousness. They looked around and saw so many new faces—some smiling, some looking just as unsure as Alex felt.
Diagnosing Pre-Diabetes
If you are showing symptoms or have risk factors for pre-diabetes, it is crucial to seek a proper diagnosis from a healthcare professional. A diagnosis will help you develop an effective treatment plan and take necessary steps to manage your condition. Your healthcare provider may conduct several tests to confirm pre-diabetes.
Physical Examinations
During a physical examination, your healthcare provider may measure your blood pressure, check your weight, and evaluate your waist circumference. These measurements can provide valuable insights into your overall health and help identify signs of pre-diabetes.
Blood Glucose Tests
Blood glucose tests are a common method used to diagnose pre-diabetes. These tests measure your blood sugar levels after fasting or a specific period. The most common blood glucose tests include:
Fasting Plasma Glucose Test (FPG): This test involves measuring your blood sugar level after fasting for at least eight hours. A blood glucose level between 100 and 125 mg/dL indicates pre-diabetes.
Oral Glucose Tolerance Test (OGTT): For this test, you will drink a sugary solution, and your blood sugar levels will be measured periodically for two hours. A blood glucose level between 140 and 199 mg/dL indicates pre-diabetes.
Random Plasma Glucose Test: This test involves checking your blood sugar level at a random time, regardless of your meal schedule. A blood glucose level of 140-199 mg/dL may indicate pre-diabetes.
Hemoglobin Glycosylated A1C test
Another test commonly used for diagnosing pre-diabetes is the Hemoglobin Glycosylated A1C (HbA1c) test. This test provides an average of your blood sugar levels over the past three months. An HbA1c level of 5.7% to 6.4% indicates pre-diabetes.
By undergoing these tests, you can receive an accurate diagnosis and understand the severity of your pre-diabetes. This information will help your healthcare provider create an individualized treatment plan to manage your condition effectively.
Treating Pre-Diabetes Symptoms
Reversing insulin resistance and preventing the progression to type 2 diabetes is possible through lifestyle changes, medication, or a combination of both.
When diagnosed with pre-diabetes, it’s crucial to take immediate action to manage your condition and reduce the risk of developing type 2 diabetes. By implementing the following treatment approaches, you can improve your overall health and well-being:
Adopt a Healthy Diet: Incorporate a variety of nutrient-rich foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats, into your daily meals. Limit the consumption of processed foods, sugary beverages, and foods high in saturated and trans fats.
Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise every week, such as brisk walking, swimming, or cycling.
Control Portion Sizes: Be mindful of the quantity of food you consume. Use smaller plates and bowls to avoid overeating and practice portion control.
Maintain a Healthy Weight: If you are overweight or obese, losing just 5-10% of your body weight can make a significant difference in managing pre-diabetes.
Monitor Blood Sugar Levels: Regularly check your blood glucose levels as advised by your healthcare provider. Keeping track of your levels can help identify patterns, evaluate the effectiveness of your treatment plan, and make necessary adjustments.
Consider Medication: In some cases, healthcare professionals may prescribe medication to help manage blood sugar levels. These medications may include metformin, which improves insulin sensitivity, or other medications that assist with blood sugar control.
Remember, managing pre-diabetes requires a long-term commitment to a healthy lifestyle. By proactively taking care of your health and following the recommended treatment approaches, you can reduce the risk of developing type 2 diabetes and lead a fulfilling life.
Taking Action for Better Health
While pre-diabetes may not always be reversible, there are steps you can take to support your overall health and manage insulin resistance. It’s crucial to listen to your body and make lifestyle changes that promote well-being.
One essential aspect of managing pre-diabetes is reducing stress. Chronic stress can negatively impact insulin sensitivity and contribute to elevated blood sugar levels. Finding healthy ways to manage stress, such as regular exercise, meditation, or engaging in hobbies, can be beneficial for your overall health.
Proper nutrition is another key component in managing pre-diabetes. Focus on a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Be mindful of portion sizes and aim to avoid sugary drinks and processed foods. A registered dietitian can provide tailored guidance and help you create a meal plan that suits your needs.
Regular physical activity is also crucial in managing pre-diabetes. Engaging in exercise such as brisk walking, cycling, swimming, or strength training can help improve insulin sensitivity and lower blood sugar levels. Aim for at least 150 minutes of moderate-intensity exercise per week, spread across several days.
To stay proactive and informed about pre-diabetes, consult your healthcare provider for personalized advice. They can guide you in developing an individualized pre-diabetes treatment plan and monitor your progress. You can also seek information and resources from trusted sources like the Mayo Clinic or the Centers for Disease Control and Prevention. By taking control of your health and implementing these strategies, you can reduce the risk of developing further complications and improve your overall well-being.
FAQ
What are the common symptoms of pre-diabetes?
Common symptoms of pre-diabetes include excessive thirst, frequent urination, fatigue, blurry vision, unexplained weight loss, and slow wound healing.
Who is at risk for pre-diabetes?
Factors that increase the risk of developing pre-diabetes include being overweight, having a family history of type 2 diabetes, being over 45 years old, having African, Latino, or Native American ancestry, smoking, and taking certain medications.
How can I recognize pre-diabetes symptoms?
Symptoms of pre-diabetes can include having a waistline over 40 inches in men and over 35 inches in women, skin tags or patches of dark velvety skin called acanthosis nigricans, high blood pressure, elevated fasting glucose levels, increased triglycerides, and low HDL cholesterol.
What tests may be conducted to diagnose pre-diabetes?
Healthcare professionals may conduct physical examinations, blood glucose tests, and the hemoglobin glycosylated A1C test to confirm the diagnosis of pre-diabetes.
How can pre-diabetes symptoms be treated?
Pre-diabetes can be managed through lifestyle changes such as adopting a healthy diet, incorporating regular physical activity, and, in some cases, medication may be prescribed to help manage blood sugar levels.
Share on Facebook